Throughout the majority of my treatment, I’ve not asked many questions about the choices I’ve been offered. NHS breast cancer treatment is fairly standardised, regardless of where you live or who you see, and every patient is discussed at an MDT to ensure that nothing is missed out when discussing treatment options. I’d heard about a trial, Create-X, whose preliminary results had just been published at a major international conference in December of last year, showing some benefit from further chemotherapy for patients, a bit like me, who hadn’t responded to their first chemotherapy.
Should I ask questions about my treatment?
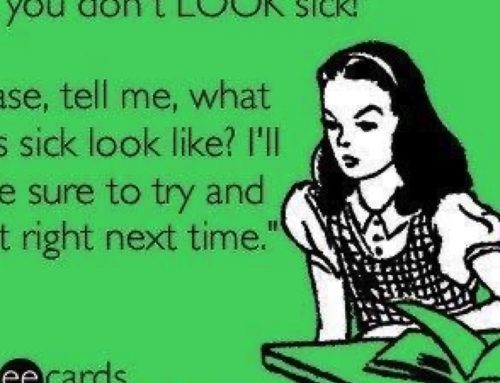
I wanted to know whether I would be suitable for more chemo (I know, I know, as if it wasn’t bad enough last time), but felt very, very awkward about asking my oncologist and surgeon. I didn’t want to be a ‘know-it-all’ patient, but if I did know something that my own doctors didn’t, was it OK to bring it up? I stressed about this for several days, and in the end spoke to my breast care nurse, who was wonderful. She said it was my body, and my right to ask questions, no matter how bad I felt doing it.
I e-mailed my oncologist in advance, and she was great and researched what was available on-line before we met. I know that I don’t know everything about breast cancer (although my husband will say I know almost everything). I find it hard to remember the details of the hundreds of trials that are well known, let alone keep up with the newest data coming out of conferences I haven’t been to. It’s also quite hard to admit to a patient that you don’t know the research they are talking about, and to then admit to yourself that the patient might have found something new, and to then go away and investigate yourself, instead of brushing them off. I felt very awkward as a doctor who potentially knew more than my oncologist, and didn’t want her to think I didn’t trust her.
What to do when you don’t hear what you want
She said that on the basis of what was available about that trial (basically, an abstract which summarises the key findings only, and a transcript of a discussion about the trial at the conference), she would stick to my original plan, which was radiotherapy and hormonal manipulation. But I was welcome to get a second opinion if I wanted. And that’s where things got more complicated.
I wanted to get an opinion from an oncologist who was ideally at that conference in the States, who would know more about it than I did, but there was no way of finding out who was there. I also, at that time, wanted to see someone who would give me more chemo, regardless of whether I actually needed it, because I had convinced myself that I had to have it. Which is completely ridiculous, and goes against every bit of evidence I use to treat patients at the moment (i.e. that hormonal manipulation is what I really needed, as shown by many, many trials). I knew one oncologist who was at the conference, who would recommend, and give me, the extra chemo, but he was based a very long way away, and it could potentially mean living way from home or an awful lot of travelling to get that treatment.
Why do you want a second opinion?
And here lies the problem with second opinions – do you go to see someone who will tell you what you want to hear (regardless of whether it is a medically sound decision), or do you go to see someone who will give you a medically sound opinion, and accept that they might say no to what you want?
Who do you see? How do you find them?
How do you find the second opinion you are after? There’s no TripAdvisor for doctors. And if there were, 50 great comments can be outweighed by one bad one. Several hospitals no longer offer NHS second opinions for cancer patients. There are many reasons for this, but one we kept coming up against was financial. There’s not really any money for the Trusts concerned, and meeting cancer treatment target times can be very tight, as several weeks can be used up looking for a second opinion, leaving possibly only days to start treatment. We were lucky in that I had time to look around, as I had already had chemotherapy and surgery, so I didn’t have a ‘ticking time bomb’ that needed to be treated within a month. We were also lucky in that we could afford to pay for a private opinion, and had the benefit of being able to ask medical colleagues, as friends, for advice. How many of the general public are in that position?
Is where I work more important than who I am?
The I Want Great Care website is a good starting point, although generally the reviews are good (which is lovely to read as a doctor as we very rarely get to hear the good about our practice, only the bad when the complaints come in). Here’s my own IWGC link. Is private better than NHS? Are doctors in recognised ‘Centres of Excellence’ such as The Royal Marsden Hospital better than those of us out in the sticks (well, Ipswich is miles from anywhere). A lot comes down to how that doctor’s personality and approach fits with you, not what they know or how clever they are or how many papers they have published. I may not get on with someone but a friend may think that doctor is amazing. Does that have anything to do with how good a doctor they are?
Shallow? Me…?
If you’re paying for a second opinion, it gets even more complicated. You don’t want to pay to see someone you don’t like (although you won’t know you don’t like them until you see them). And do you want to pay someone to tell you “No”? And is an older, more experienced doctor going to be better than someone at the beginning of their career? Are years and years of experience better than up-to-date knowledge and maybe being more prepared to take a risk and try new things..? Where do you start? Does a slick website mean they are a better doctor? Is it a bit like the shallow world of internet dating, when, for me, if I didn’t like the photo then I wouldn’t ‘click’ on that person. Having an online media profile can be so important now that smart phones give us instant access. I’ll openly admit to not using a business if the website is shoddy.
I find it very difficult when patients ask me who to see for a second opinion, or who to see privately (I don’t do private practice). So far, I’ve always politely refused to recommend a name. I’ll give them tips on how to find someone, such as googling the various private hospitals’ websites, and then googling the surgeons they’re interested in, but I don’t feel I can recommend someone myself. For all of the above reasons.
Back to me…
My first thought was to find someone who would give me more chemo, despite saying that I never wanted to go through chemo again. And then the other side of my brain would kick in and I’d tell Dermot that I wanted to see an expert who would give me a sensible answer. The next day, I’d be back to wanting to see someone who would give me chemo. It’s very hard to think rationally when you’re in the middle of it all, and I must have been impossible to live with. Eventually, we decided on a sensible opinion. I had a couple of recommendations, and in the end I went with a lovely man who the oncologist where I work often refers people to. But I had wasted so much emotional energy getting to that point. However, I am glad I did. I can now understand some of the thought processes of my own patients, and can hopefully get to the real reason they are seeking a second opinion.
Some of my ladies come asking for referral for alternative treatments such as juice detoxes, or coffee enemas instead of chemotherapy, or they decline radiotherapy because they’re heard it will give them cancer. These are much harder to talk about. Breast cancer has one of the largest evidence bases, with hundreds of trials that prove that the treatment we offer works for the majority of cases. Sadly, we all know there are exceptions, and there is a lot we still don’t know. But there are no trials comparing alternative medicine or homeopathic treatments with standard cancer treatments. I will never force treatment on a patient, and it is up to her (or him) to decide what is right for them. I think my job is to make sure they know the possible consequences of going it alone and declining standard treatment.
The voice of reason
The second oncologist we saw was lovely, and because I’d e-mailed him in advance about the trial, and all my other questions, he’d had time to do his homework. Basically, he agreed with the scientist and surgeon in me, and my own oncologist. It did not make sense to give a patient (me) more chemo (with a risk that it might kill me), based on the scanty details in the abstract. Until the full trial data was published, with the exact tumour details of the women who had benefitted, and ideally until it had been repeated in another country with the same results, it wasn’t worth the risk to my health. Hard to hear, but I knew he was right.
What my cancer needed, and needed quickly, was hormones. Because the lobular cancer hadn’t shrunk during chemo, it effectively hadn’t been treated since I was diagnosed back in July, and he recommended that I start Tamoxifen and Zoladex before the radiotherapy, rather than wait till afterwards. So here comes the run…