Before I was diagnosed with breast cancer, I didn’t really think about my own mortality. I dealt with the mortality of others on an almost daily basis at work, and it takes a lot of tact and patience to talk about this with patients. With a lot of my patients, “How long have I got?” is the first thing they ask me when I tell them they have breast cancer.
Is a guess better than nothing?
During my medical training, I was often asked by patients to tell them how long they had left. I soon leaned that the right answer is ‘vaguely specific’. If you tell a patient and their family that they have a month to live, and they suddenly die within 2 days, the family feel cheated and are angry with you. On the other hand, you could tell a patient they have a month to live, and yet they live for another 4 years. Cue more anger and frustration.
I’ve just read a brilliant book by the American neurosurgeon Paul Kalanithi, who was diagnosed with inoperable lung cancer, called ‘When Breath Becomes Air’. His oncologist refused to tell him how long she thought he had left to live, and he became increasingly frustrated. He tells us why it was so important for him to know, and forgive me, I’m paraphrasing here. If he had months, he’d rest. If he had a year, he’d write. If he had 10 years, he’d go back to neurosurgery.
What to do with the days you have
When you’re diagnosed with cancer, you hear a lot of cliches about living every day as if it’s your last, don’t take anything for granted, life’s too short etc , etc. But how do you now what to do with your days when you don’t know how many you have left?
Back to breast cancer
As I was saying, the majority of patients have a very good prognosis (although there are exceptions to every rule, and I’ve seen my share of heart-breaking cases). Lots of trials have looked at survival after breast cancer – some with 20 years’ of follow-up data, and this means we are very good at predicting what a patient’s survival from breast cancer might be.
My life is made even easier because of the NHS PREDICT programme that has collated UK breast cancer data, and is very simple to use. You enter details about the patient and their tumour and it produces a 5- and 10-year survival, with and without recommended treatment.
Please think carefully before looking at the websites I mention if you’ve been treated for breast cancer. I’d hope that your oncologist or surgeon has given you this information, but I would hate for you to see this for the first time when you’re alone at home. However, I believe patients should be empowered and have access to information like this, and I found these sites on a simple Google search.
PREDICT example for a 60year old woman with a screen-detected 3cm Grade 2 tumour with clear lymph nodes that was sensitive to oestrogen.
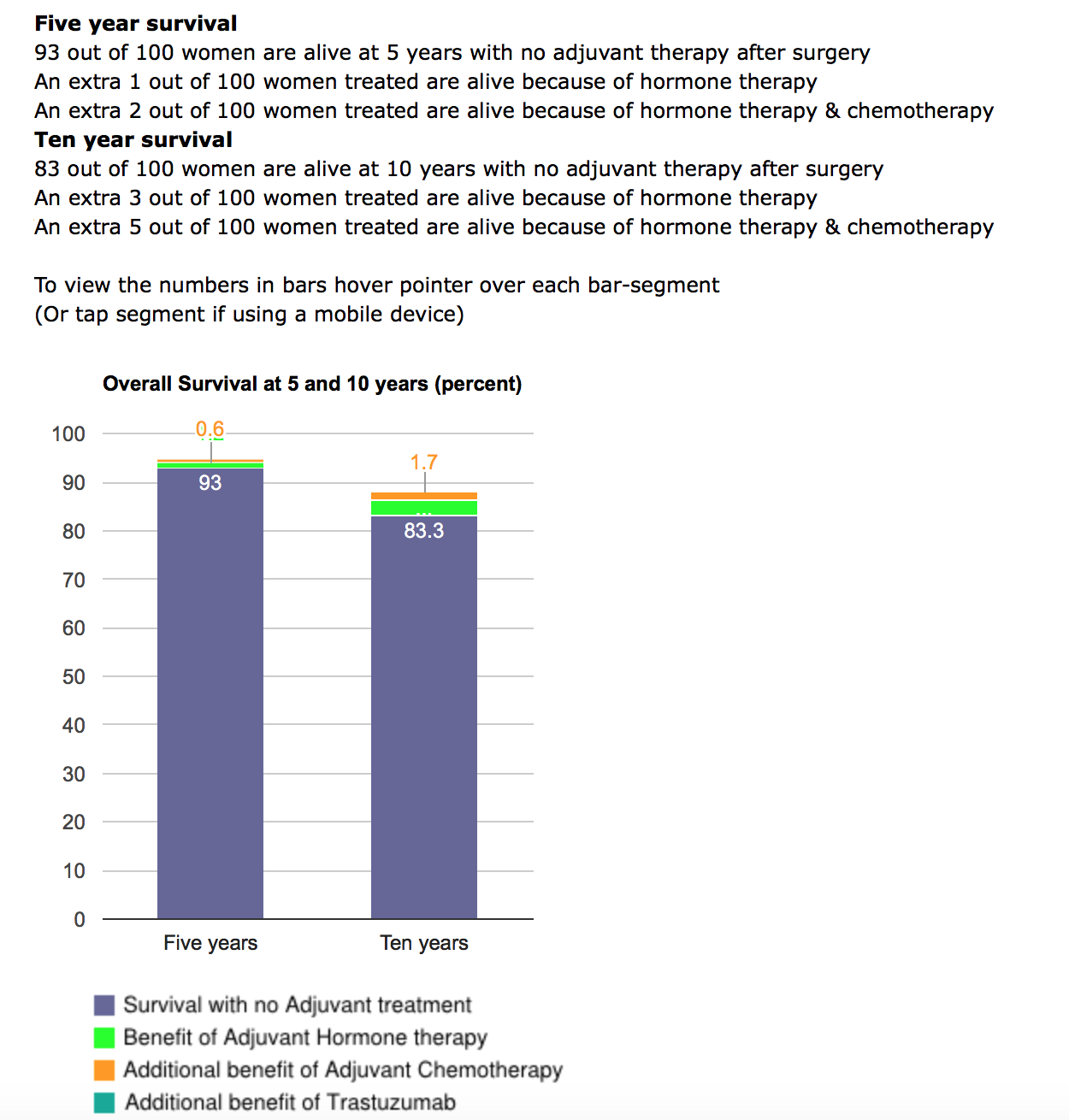
Being able to show this to a patient is a very good way of alleviating anxiety. It does have limitations, and it’s not designed for women, like me, who’ve had chemotherapy upfront. We use it in our MDTs to help decide whether a patient should be offered chemotherapy.
How long do I have?
Since I discovered that my cancer was larger than expected, and that it had spread to the lymph nodes in my armpit, I was desperate to find out how long I had. But no-one would tell me. Or was it because they couldn’t tell me, since PREDICT wasn’t fit for purpose? After doing a bit of ‘Googling’ I found a Chemotherapy Response Calculator on the MDAnderson Cancer Centre website. It’s not designed for women who had Taxane chemotherapy like me, and my prognosis wasn’t great.
The only other alternative is the Nottingham Prognostic Index. This is basic, but has been shown to be equivalent to Adjuvant Online! (an American breast cancer prognosis tool) in this study. When I put my numbers in, it placed me in the worst prognostic group (<50% chance of 5-year survival). But as I’ve said before, treatments are improving all the time, and like PREDICT, it wasn’t designed for women who had chemo upfront. I plan on living for a very long time, regardless of what the numbers say.
I did put my numbers into PREDICT to see what might come up, but once I went above 50mm in size, the numbers stopped changing. I think it’s because there are relatively small numbers of women with large tumours, so that the data isn’t available to accurately predict our survival.
Now what?
I had a sudden awareness that I might not live forever (as stupid as that sounds now). I needed my husband to acknowledge that I might die before him, even though he’s 10 years older than me, and that it might be sooner than we both thought.
The problem with being given a number – for example, an 85% chance of being alive in 10 years, is that, for you, the number is irrelevant. It’s not 85:15 chance of being alive, it’s actually 1:1. You either die because of your cancer, or you don’t. You either die early, or you don’t. You could be the exception that outlives all your doctor’s predictions and are still alive at 30 years when they gave you 5, or you could be the exception that obeys none of the rules and dies way before your time. There is no way of knowing with absolute certainty. And so I’m back to living my life, one day at a time.